The Five Elements of Optimal Care Delivery

Our country’s healthcare system is in the throes of transformation. While the move to value-based care is positive and much needed, providers are confronting formidable challenges to re-engineer how they’re delivering care, while facing the added pressure of taking on financial risk. In an environment driven by new policies and regulations and an increasingly competitive market, all roads lead to establishing a high-value network. But many providers are asking the same question – where do we begin?
Value = Differentiation
In today’s market, a health system succeeds by setting itself apart and becoming the provider of choice among consumers. High-value care is key to differentiation among competitors, and achieving care delivery optimization is the foundation of high-value care. Equipped with experience and lessons learned over the past two decades of working with some of the nation’s leading hospitals and health systems, Premier® has developed a performance improvement framework with the five strategic elementsgovernance structure of optimal care delivery.
In a new guidebook, Premier experts take a close look at each element. In this blog series, we’ll offer additional insights on how to invest in and foster a culture of care delivery optimization.
Let’s start with the basics and an introduction to the framework.
Care Delivery Optimization Framework: A Snapshot
Premier’s framework can be characterized as a five-phased roadmap to guide health systems in the creation and implementation of optimal care delivery that is both affordable and sustainable.
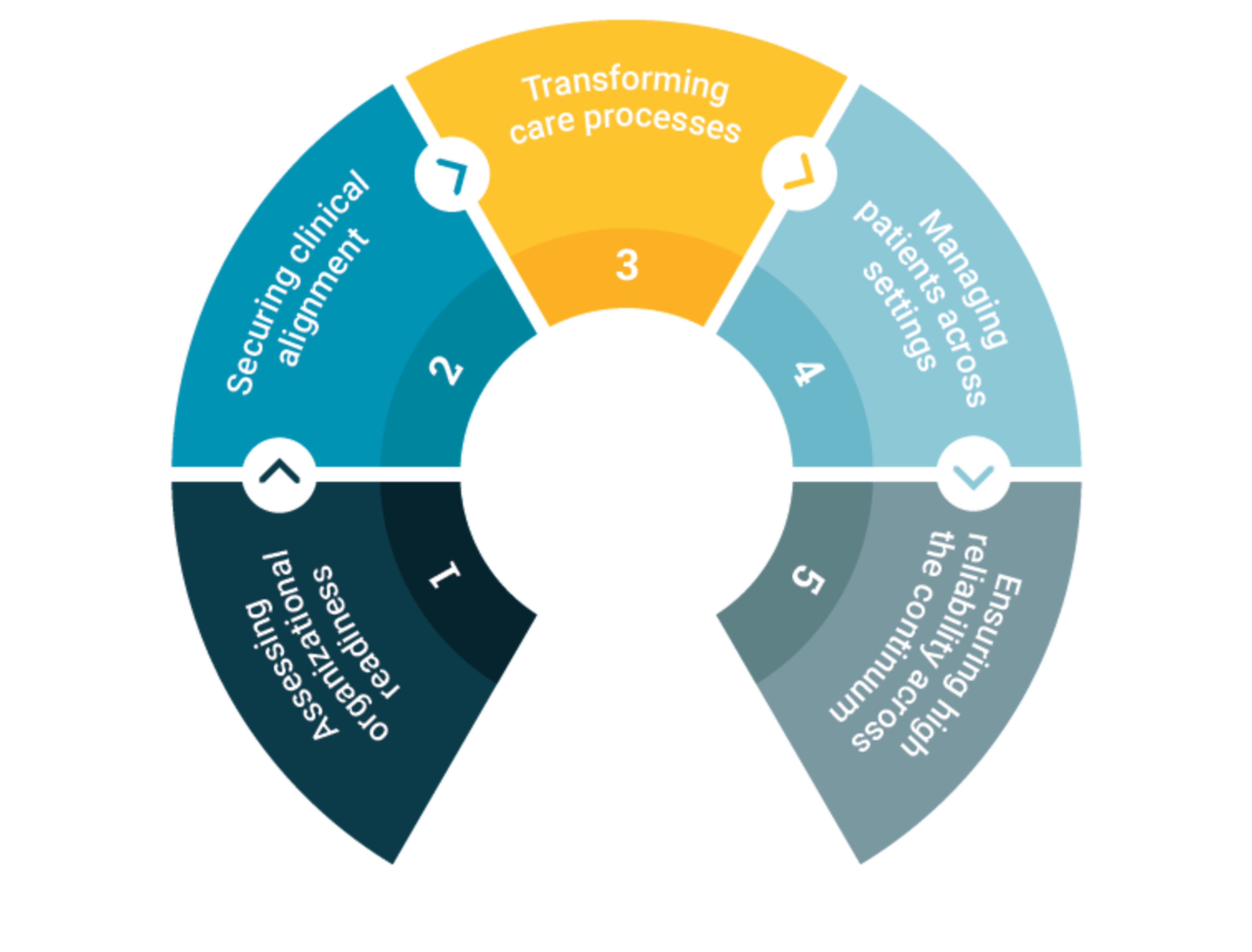
1. Assessing Organizational Readiness
The first step is to complete a comprehensive assessment of the current state of play and the pathway toward achieving future goals. This includes a formal readiness assessment to identify an organization’s strengths, weaknesses and areas of opportunity, and examine institutional finances to determine what investments are feasible. In addition to having strong leadership and commitment among the C-suite, clinical leaders and other administrators, it is critical for health systems to have a clear governance structure that delineates roles and responsibilities. During this initial phase, designated leaders need to leverage available data to understand cost, quality and outcomes patterns, and begin identifying priority areas for clinical and operational redesign. The key to understanding potential opportunities is to compare and benchmark data against peers.
Fostering a culture that embraces change, improvement and accountability may be the biggest challenge. Promoting this type of culture includes implementing training programs and transparent communication of progress and deficits through dashboards and scorecards.
2. Achieving Clinical Alignment
Hospital alignment and collaboration with physicians is imperative. Engaging physicians as partners and leaders is necessary for successful buy-in and execution. Physicians must be at the table to weigh in on decisions and goals, and lead clinical transformation efforts. Physician partners should have a clear understanding of quality and cost goals and the metrics being used to measure their performance. Additionally, financial incentives must be aligned with improved care delivery practices, while transparent communications must be implemented so that physicians clearly understand how their performance affects compensation.
3. Transforming Care Processes
To drive sustained success, providers should develop and deploy evidence-based clinical care pathways across the care continuum. Best practices of evidence-based care include the use of checklists, frequent and timely feedback to clinicians, daily reviews of patient records, and the use of multidisciplinary teams, among other protocols. Successful health systems have easy access to robust patient, performance and operations data, along with analytics systems in place to effectively use this information.
4. Managing Patients Across Settings
A whole-person, patient-centric approach employs the use of care managers as a “home base” for patients to promote coordination across multiple settings of care, minimize duplicative services and facilitate transitions. Communication should be face-to-face as much as possible, and documentation must be meticulous. To cultivate a system that prioritizes population health management and accountability, clinical surveillance technology should offer customizable reports, comprehensive pharmacy management tools, and reporting systems configured to align with federal and state regulatory requirements.
5. Ensuring High Reliability Across the Continuum
Improvement is only meaningful if it’s sustained. The ultimate goal is for health systems to become high-reliability organizations and practice continuous monitoring and performance improvement to promote organizational awareness, accelerate change and strive for excellence.
In the next blog of this series, we dive deeper into assessing organizational readiness, paying particular attention to the importance of fostering a data-driven culture that embraces open communication and shared accountability.
To learn more, download Creating a Culture of Optimal Care Delivery or contact us.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.