Premier, Inc. Data: More Than 86 Percent of Providers Experiencing Shortages of IV Fluids in Aftermath of October Hurricanes

Key Takeaways:
- New Premier survey data shows that more than 86 percent of U.S. healthcare providers nationwide are currently experiencing IV fluids shortages in the aftermath of Hurricane Helene.
- This data also shows that providers are starting to cancel procedures and more may follow suit in the next month if the situation doesn’t improve.
- Smaller providers (those with 25 or fewer beds) were more likely to report receiving zero percent of their ordered quantities of IV fluids.
- Conservation procedures as well as alternative strategies to help accelerate production remain critical as providers are concerned shortages could spill over into other product categories and the situation could worsen in the aftermath of Hurricane Milton.
New provider survey data from Premier, Inc. finds that more than 86 percent of healthcare providers are experiencing shortages of IV fluids in the aftermath of Hurricane Helene. Shortages were evenly spread nationwide, across all provider types. Shortages also seemed to evenly affect providers regardless of size or system affiliation.
IV fluid supply first became compromised after the primary manufacturer with more than 60 percent market share in the United States sustained damage at its North Carolina facility as a result of Hurricane Helene.
Of the Premier survey respondents, 88 percent report they are receiving less than half of their requested orders for IV fluids. As a result, approximately 54 percent of respondents have 10 days or less of IV fluids in inventory, down from a more typical supply of 15 to 22 days on hand, according to historical Premier purchasing and real-time ordering data, with limited ability to replenish those stocks. Smaller providers (those with 25 or fewer beds) were more likely than other types of providers to report receiving zero percent of their ordered quantities of IV fluids.
Considering these trends, providers reported in qualitative survey comments that it’s only a matter of time until supplies dwindle to zero.
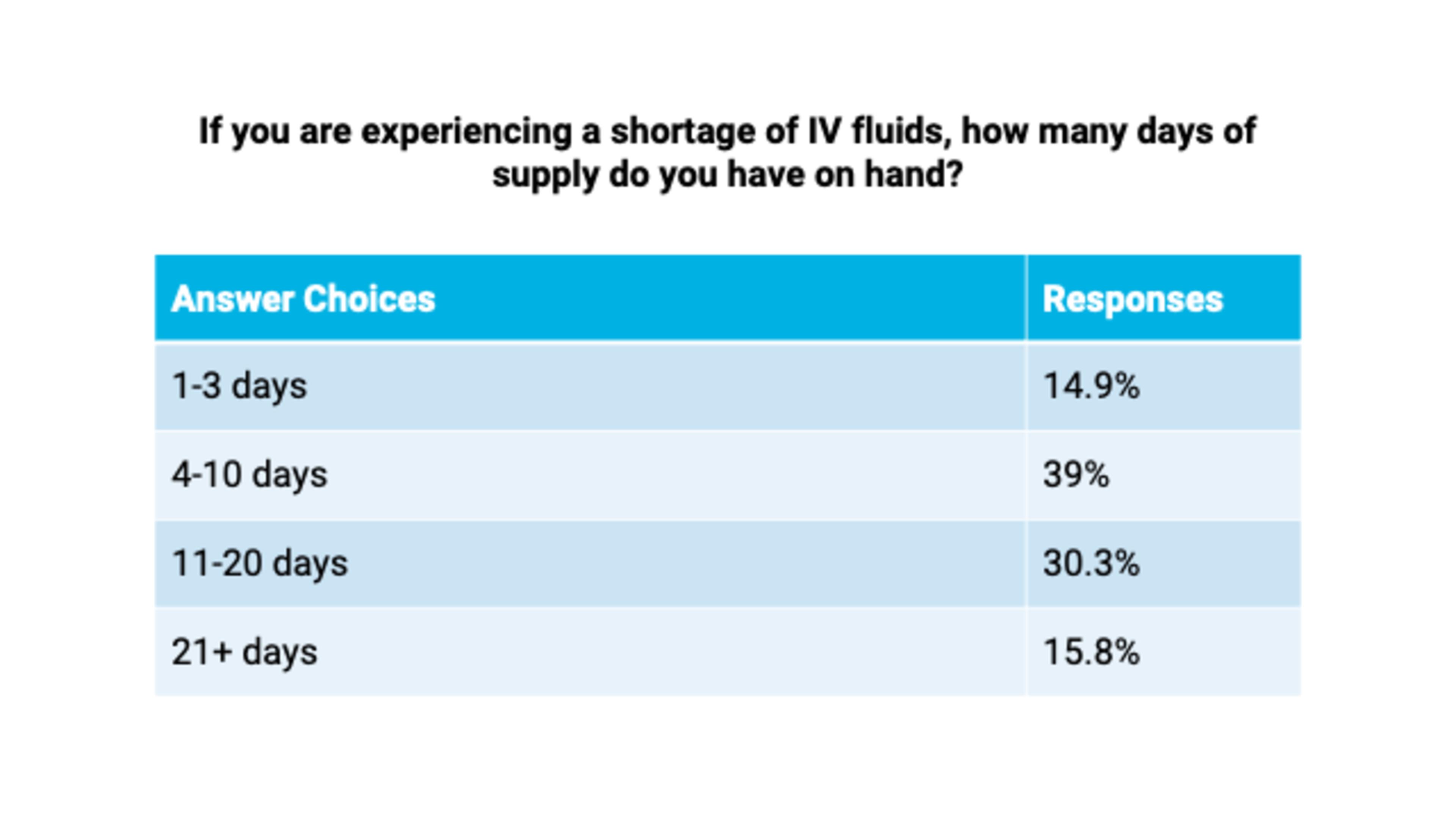
Source: Premier IV fluids member survey (October 7-October 8, 2024). 228 respondents.
Given limited product availability, nearly 17 percent of surveyed providers have cancelled elective surgeries and other procedures, and another 58 percent are considering that option in the near term. In addition, 78 percent of providers report that they will be forced to consider cancelling procedures in the next month if the situation does not improve.


Source: Premier IV fluids member survey (October 7-October 8, 2024). 235 respondents.
To stretch scarce supplies, more than 81 percent of respondents have implemented conservation protocols for IV fluids.
Spillover Effects
Nearly 60 percent of respondents are most worried about how long the current shortage will last, with another 25 percent reporting that finding alternative sources of supply was their primary concern, according to Premier’s survey.
These concerns come into greater focus considering that even while the North Carolina manufacturing plant begins its recovery efforts, the second largest manufacturer of IV fluids in the United States sits in the path of Hurricane Milton, which many are predicting to evolve into a “once in a lifetime” disaster event.
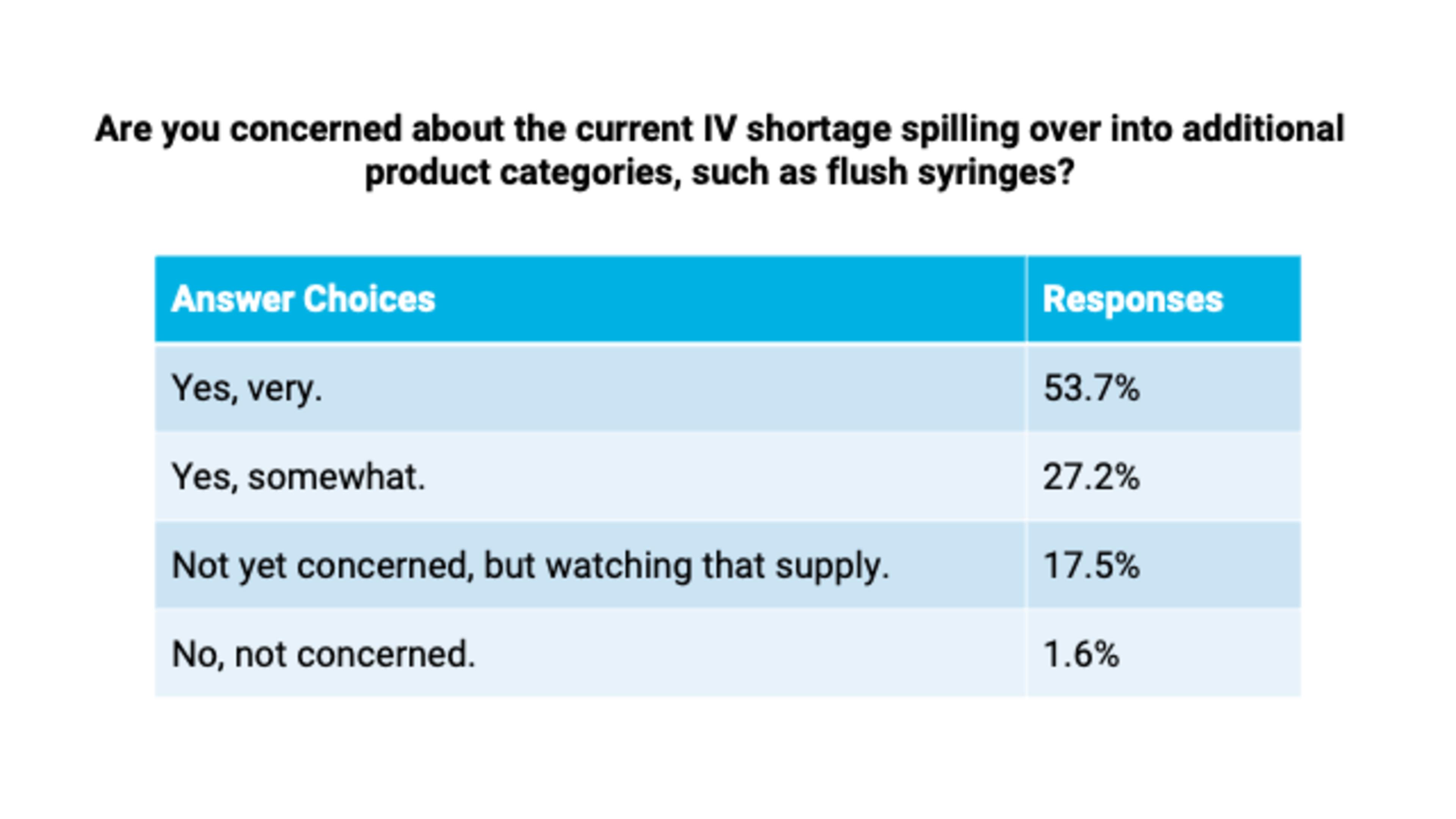
Should the market experience back-to-back events compromising the production capabilities of the two largest IV fluids manufacturers, more than 80 percent of provider respondents said they were concerned that shortages could exacerbate and spill over into other product categories, such as flush syringes, sterile water, IV bags and tubing, oral hydration solutions and other supplies used in daily patient care.

Source: Premier IV fluids member survey (October 7-October 8, 2024). 257 respondents.
In addition, more than 40 percent of providers reported that they had started receiving solicitations from unapproved, gray market suppliers offering to sell them IV fluids at highly marked up prices, raising additional concerns about price gouging and product authenticity at a time when many are struggling to obtain products necessary for routine operations and patient care.
Source: Premier IV fluids member survey (October 7-October 8, 2024). 255 respondents.
Premier continues to prioritize hurricane preparedness and response actions, including the management of IV fluids supply. Together with our members, manufacturers, government officials and other supply chain stakeholders, Premier teams are working around the clock to help mitigate any potential effects to healthcare operations and the delivery of patient care.
Leading Advocacy Efforts
Armed with this survey data, Premier continues to advocate for action by the federal government to ensure healthcare providers have a sufficient supply of IV fluids to care for patients. The Premier team has:
- Coordinated with the Food and Drug Administration (FDA), Department of Health and Human Services (HHS), Administration for Strategic Preparedness and Response (ASPR), White House, and other federal agencies to help keep them updated and educated on the current state of play.
- Escalated the need for the FDA to add all impacted IV fluids to the FDA drug shortage list so they can evoke statutory authorities under 21 U.S. Code § 356c and other provisions to expedite inspections, approve alternate manufacturers, import product as necessary, leverage 503B compounding as an interim solution, extend expiration dates, and pursue other opportunities to mitigate impacts to patient care.
- Urged the FDA to share, from their perspective, the extent of remediation required at the impacted facility and the level of effort needed to resume production such that the industry could better understand the anticipated timeframe of the shortage.
- Confirmed that the Strategic National Stockpile (SNS) does not maintain an inventory of impacted IV fluids.
- Met with the White House Supply Chain Team to discuss mitigation strategies and opportunities for public-private partnerships to help address the shortages, including potentially leveraging the Defense Production Act or a military air bridge to bring available product from overseas.
- Coordinated with other D.C.-based advocacy organizations to align on messaging and share critical insights with federal partners.
- Coordinated with the Centers for Medicare & Medicaid Services (CMS) to recommend accelerated payments to Medicare Part A providers and advance payments to Medicare Part B suppliers in Federal Emergency Management Agency (FEMA)-designated disaster zones to alleviate cash flow issues caused by the disaster.
- Continued to advocate for the FDA to fully implement statutory authority Congress granted it in March 2020. For example, Congress directed FDA to require contingency and redundancy plans from manufacturers, but FDA has yet to finalize guidance in this space, and therefore, manufacturers are not required to submit their resiliency plans at this time.
Premier’s survey data underscores the need for Congress and federal agencies to leverage recent learnings and respond with a cohesive national strategy to help support and stabilize the U.S. supply chain in the long-term for better preparedness during emergencies.
To this end, Premier continues to advocate for legislation such as The Medical and Health Stockpile Accountability Act (H.R. 3577) that if implemented, would have helped our nation identify available inventory of IV fluids on U.S. soil to develop dynamic allocation processes, better understand the extent of shortages, and identify needs to ramp up capacity and production by alternate suppliers.
This legislation will stand up a national automated data collection infrastructure that can track critical product availability across the entire supply chain in near real-time during emergencies. A data-driven supply chain infrastructure will also provide real-time intelligence to inform future policymaking during times of emergencies, such as leveraging the Defense Production Act to ramp up supplies so that the healthcare system isn’t caught short-handed.
Solutions for Risk Mitigation and Resiliency
Alongside advocacy efforts, Premier continues to act as a trusted connection point for healthcare providers, manufacturers and the government – working 24/7 to address challenges in real-time and help providers across the nation access the supplies they need to serve their communities. We are also partnering across the private sector to create both short-term and long-term solutions, sharing our insights to help inform public understanding, specifically:
- We’ve established a daily touch point internally to review employee, member and supplier status updates, needs and potential impacts as a result of the storms.
- Premier experts continuously collaborate to share IV fluids conservation strategies – providing ongoing guidance for providers to reduce fluid shortage workarounds and support greater efficiency. Conservation of existing IV fluids products in the supply chain remains the primary means of disruption mitigation at this time.
- Premier is exploring alternative options to help strengthen the IV fluids market, including:
- Working with current suppliers to determine inventory levels and strategies to maximize production capacity.
- Collaborating with government agencies to expedite approvals and import options for overseas suppliers.
- Identifying regional compounding facilities and new manufacturers to assess timelines and accelerate IV solutions production.
- Premier’s Supply Disruption Manager helps providers identify potential product shortages in advance – with over 90 percent accuracy – and recommends clinically approved equivalent products. Alongside benefits to providers, Supply Disruption Manager helps suppliers adequately plan production and inventory management, anticipating demand spikes and preventing shortages.
- Our Disaster Preparedness and Response team offers dedicated support during a hurricane or other emergency – providing real-time information and key resources to help minimize impacts to the supply chain and patient care. Additionally, Premier’s Disaster Preparedness contract category includes suppliers certified in emergency response and restoration activities for impacted members.
Premier will continue to work directly with our members and other stakeholders on this dynamic situation. For any emergency needs, Premier members can reach out to region leaders or email DisasterResponse@premierinc.com.
Methodology
Premier fielded the survey among its provider members from October 7-October 8, 2024. Respondents included 257 providers, 90 percent of which staff acute care beds, 37 percent with non-acute beds, 33 percent with surgery centers and 29 percent with physician offices and other settings of care. Note that some respondents have assets in all surveyed categories, so results do not total 100 percent. In total, respondents represent 101,143 patient beds – about 11 percent of the total acute care beds in the nation. Respondents included 24 percent from the Southeast, nearly 8 percent from the South-Central region, 10 percent from the Southwest, 33 percent from the Northeast, 26 percent from the Midwest and 10 percent from the Northwest. 30 percent of respondents were small providers (60 or fewer beds) and 30 percent were large (250+ beds). Not every respondent answered every question. Premier did not independently verify respondents’ self-reported results.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Andy leads the acute and non-acute field and sales teams, Premier’s sponsor programs, commercial operations, Nexera consulting and co-management functions, as well as the stockd® e-Commerce and alternate site business.

With 15 years of diverse supply chain strategy and operations experience, Kyle leads Premier’s supply chain business process improvement initiatives and has executive leadership responsibility for Premier’s Supply Disruption and Disaster Preparedness and Response efforts.
Article Information

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Andy leads the acute and non-acute field and sales teams, Premier’s sponsor programs, commercial operations, Nexera consulting and co-management functions, as well as the stockd® e-Commerce and alternate site business.

With 15 years of diverse supply chain strategy and operations experience, Kyle leads Premier’s supply chain business process improvement initiatives and has executive leadership responsibility for Premier’s Supply Disruption and Disaster Preparedness and Response efforts.